Blazevich et al in the most recent issue of the Journal of Applied Physiology have an article that examines what happens on several levels as a result of three weeks of flexibility training for the ankle joint. In future years, we may be looking back at this study as one of those profound studies that change the way we think and practice. I wanted to cover this study because it can be read on one level (here’s the study, here’s the results), but I think it’s worth spending a little time covering some of the implications.
In this study, subjects were trained twice a day for three weeks. The training consisted of four, thirty second calf stretches against the wall (i.e. hold the wall, put the foot to be stretched behind you). The authors looked at the properties of the muscles, properties of the tendons, as well as neural activity.
Results:
- After three weeks of training, subjects increased their range of motion increased by almost 20%.
- Training did not change EMG amplitudes at the soleus or gastrocnemius.
- Training did not change spinal motor neuron excitability at the soleus or gastrocnemius.
- Fascicle and whole muscle length increased as a result of training during a maximal tolerable stretch. Fascicle length increased by over 22%, muscle length by over 12%. This coincided with a decrease in tendon strain by almost 20%.
- At the same time, at stretch termination (i.e. end range-of-motion) the training resulted in no change in tendon length while there was a 13% increase in muscle length.
So, one way to look at this study is that three weeks of flexibility training made the subjects more flexible. What is interesting is when you look beyond that obvious result. The authors suggest that the above shows that the muscle undergoes an increase in its passive elasticity, while at the same time the tendon’s stiffness is unchanged. This is really interesting, but I’ll talk a little more about this later. The authors cannot find a change in muscle activity as a result of stretch training, this includes muscle recruitment patterns as well as spinal motor neuron excitability. In other words, gains from stretching are not a result of learning how to “quiet” the nervous system. The changes in fascicle and muscle lengthening versus tendon strain/length suggest that stretch training acts differently on the muscle and the tendon.
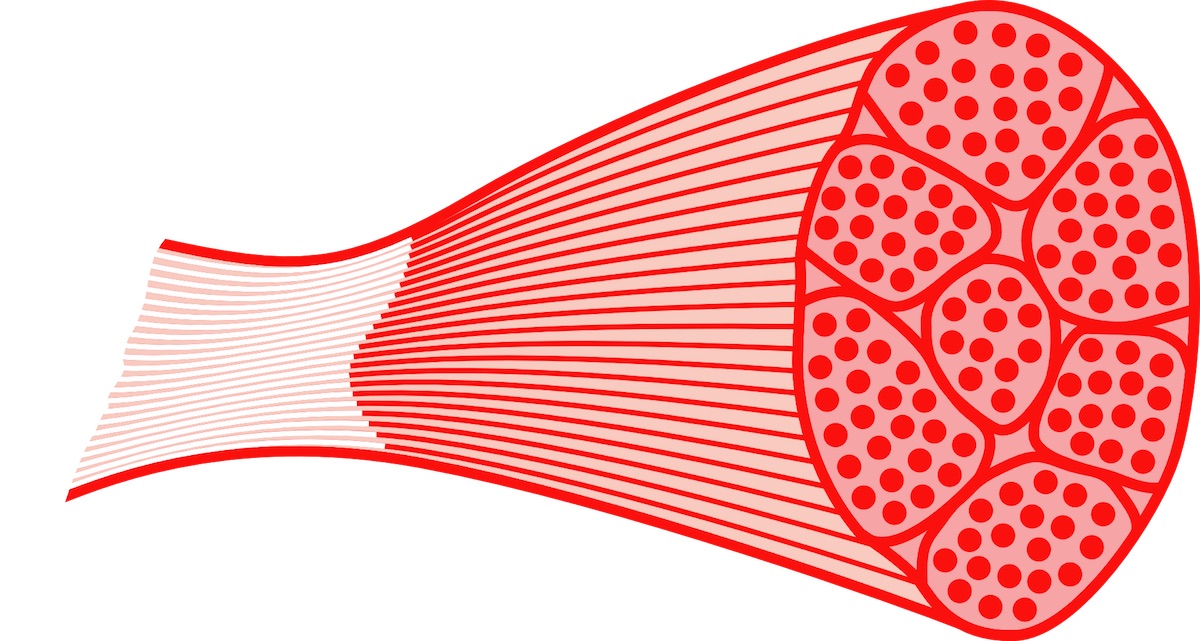
Why is this information important? First, it suggests that stretch training may not be enough to change the properties of the tendon. In other words, if you are performing a lot of flexibility work to train your tendons, rehab tendon injuries, or prevent tendon injuries then you may be wasting your time. Second, some of the adaptations to stretch training may be occurring in the three layers of connective tissue (endomysium, perimysium, and epimysium) that surround muscles, fascicles, and muscle fibers. Third, if true this information suggests that using flexibility training to “quiet” overactive muscles isn’t going to work (i.e. since there is no neural effect). While this is only one study, while its purpose was not to look at that, and while this is only my opinion it may eventually call into question some common assumptions in exercise programs.
I’m going to temper this last thought by pointing out that this was a study looking at the impact of a consistent, three-week long stretching program. It was not a study detailing how stretching impacts athletic performance. However, these findings may provide some insight into why “stretching as warm-up” has a negative impact on power activities; stretching may change the passivity of the connective tissue of the muscles so that these tissue allow a greater elongation. Maybe stiffness (as opposed to passiveness) is required for the elastic energy that is important for sprinting, jumping, throwing, etc.
Blazevich, A.J., Cannavan, D., Waugh, C.M., Miller, S.C., Thorlund, J.B., Aagaard, P., and Kay, A.D. (2014). Range of motion, neuromechanical, and architectural adaptations to plantar flexor stretch training in humans. Journal of Applied Physiology, 117: 452-462.